| |
|
|
| |
|
UNDERGRADUATE
Undergraduate Work
- Curriculum is based on a more vertically and horizontally integrated model with more clinical input from inception.
- students in the first, second and third years apart from the fourth and final years particularly promoting
- Problem based learning
- Self learning
- Community oriented learning
- formative and summative assessments
Teaching / Learning Methods
- Lectures
- Use of technology in education ; IT
- Actively promote an environment with opportunities for self learning, self direction and self discipline.
- The motivation amongst students is maintained by appropriate assessment at the end of appointment and course
Teaching / Learning Activity
Year 1
Y1S1
- Blood & Circulation/Respiration & Gas exchange module
- Lecture – Basic Life support
- Practice sessions – 03 sessions
Year 2
Y2S1
- Nervous control, Behaviour & Special senses module
- Seminar – Physiological, clinical and psychosocial aspects of pain
Y2S2
- Integrated Applied Medicine 1 – Student seminars and integrated discussion
IAM Module
Objectives 
Time Table 
Year 3
Introductory programme for the clinical
- Lecture- Emergency Life support
- Practical session - Emergency Life support
- Skills training
Year 4
Lecture Topics
- Introduction to Anaesthesia
- Drugs used in General Anaesthesia & Regional Anaesthesia
- Medical disorders & Anaesthesia I
- Medical disorders & Anaesthesia II
- Preoperative patient assessment & preparation
- Regional Anaesthesia
- Post operative care & complications
- Monitoring techniques I
- Monitoring techniques II
- Respiratory failure & Management
- Shock
- Fluid and electrolyte balance
- Intra Venous fluids & Parenteral Nutrition
- Assessment of blood loss and blood transfusion
- Oxygen Therapy
Y4S2 Integrated Applied Medicine 2 – Student seminars and integrated discussion
Assessments
Year 1
Summative assessment
Practical question on BLS –Y1S1 OSPE B Practical Exam
Year 2
(integrated module)– Summative assessment
MCQ, OSCHE
Year 3
Formal assessment of History taking
Year 4
NONE
Year 5 - Lecture Topics
- Trauma I
- Trauma II
- Management of Head injuries
- Emergency Management I
- Emergency Management II
- Respiratory function tests ABG
- Acid base abnormalities
- Cardiac Support and Inotropes
- Respiratory support including mechanical ventilation
- Acute Renal Failure
- Sepsis
- Fluid management in different conditions
- Management of Pain
- Acute Liver Failure
- Transport of Critically ill
- Ethics in Critical Care & Anaesthesia
- Management of unconscious patient
- Anaesthesia Questions
- Critical Care Questions
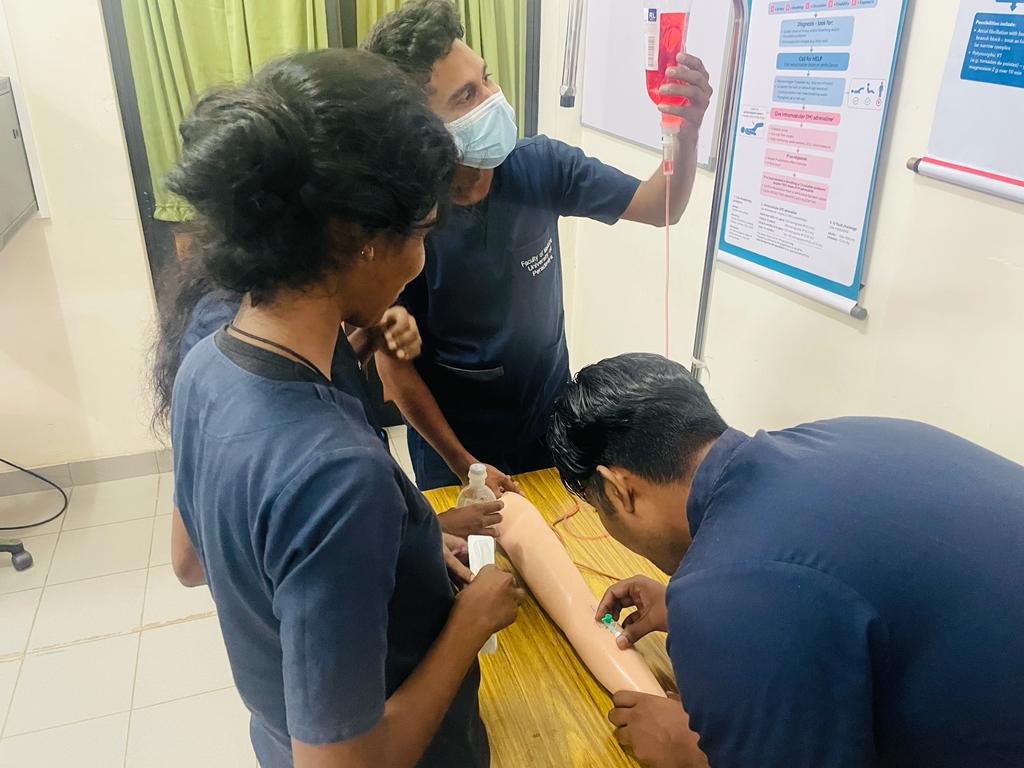
Year 5 - Clinical Appointment
- The students are allocated to small groups (3-4 in each) and rotated to various assignments within hospital with clear objectives of learning.
- The clinical placements
- THP- Intensive Care, Operating Theatre Emergency Treatment Uni
- THK - Operating Theatres Cardio Thoracic Unit, NeuroSurgical Intensive Care Unit, Surgical Intensive Care Unit and Dialysis Unit
A comprehensive student log book is provided to ensure they undergo thorough training on clear objectives of both anaesthesiology & Critical Care. Each group is exposed to formal teaching course in Cardio Pulmonary Resuscitation. In the afternoon activities include small group discussions, teaching/learning with simulation at Skills Lab and Ward teaching.
Year 5
1 month of clinical practice - 260 hrs.
5 week days 7.30am-12noon & 2.00pm-8.00pm ; 10.5x5x4 = 210 hrs
Saturday- 7.30am-12noon ; 4.5 x 4 = 18
Sunday- ( Casualty Day) 2.00pm-10.00pm 8 x 4 = 32
Total hours 260
Compulsory 80% attendance
Contents of Log Book
- Attendance
- Daily Schedule
- Objectives of the Assignment
- Essential knowledge : Anaesthesiology
- Essential knowledge: Critical Care
- Essential Clinical Skills: Critical Care
- Topics to be covered as small group discussions
- OSCE and the pass marks
Skills to be achieved during the clinical appointment
- CPR
- Endotracheal Intubation
- NG Tube insertion
- Venesection
- IV Cannulation
- Transfusion
- Blood gas analysis
- CVP measurement
- Chest physiotherapy
- Airway management in recovery
- Ambu ventilation
- Setting up ventilator
- Urinary catheterization
- IV drug administration
- Priming IV lines without air bubbles
- Taking a 12 lead ECG
- Setting up an infusion pump
Teaching methodology
- Lectures
- Student seminars
- Clinical training program
- Skills training – during clinical appointment
- Simulation mannequin skills lab
- Direct observation of procedural skills
- Case based discussions in the theatre & ICU- on a schedule
- Bedside Teaching
- Practise viva sessions within the student group
- Practise of setting of question method within the student group
- Short student presentations
- Interactive sessions
- Student centered teaching
- Pre-op Assessments and critical care admissions
- Case Presentations
Formative assessment – OSCE
- Objective Structured Clinical Examination (OSCHE). 3 mi
- Five questions until 1017 changed to 10 from 2018
- Blue print
- Emergency
- Calculation
- Identification of equipment
- Data interpretation
- Clinical decision
- Obtained 50% pass mark at the end of appointment
Summative assessments
Year 5 final MBBS
- MCQ – 4 (MCQ,SBA)
- Theory ; SAQ – 1
- Viva (10 min )
- OSCE 1-2 (1 Min each )
Marking scheme
- MCQ- Common MCQ All island
- SAQ
- Setting question based on the department decision on rotation
- Double marking by the owner of the question and nominee by the Head (Combination of internal and external examiner )
- Marks 50/100
- Viva – 10/10
- Two examiners
- Marks 10/10
- OSCE – 1 Each
Scrutiny and Result
- Scrutiny
- At departmental level (Anaesthesia and CC followed by dept of surgery )
- At Faculty level
- Results
- Pre results board at Dept. of Surgery
- Results board FOM
Examiners
- Internal
- External
- Approved at the department and faculty level










Year 1 Semester 2 BLS Practical






|
|
|
|
|
|
|
 |
|